- Included below are all Tables and Figures we refer to in ECG Blog #42. By offering them separately here - We hope to facilitate side-by-side viewing as you read through Blog 42. (Please also check out the relevant PDFs we provide links for below for full interactive discussion and more on the differentiation of WCT Rhythms):
==========================
.jpg) |
| Figure 1: 12-lead ECG obtained from a patient whose BP was dropping. Click HERE to return to ECG Blog #42. |
==========================
==========================
 |
| Table 2: After applying Table 1 (ie, "Assume VT until until proven otherwise) - we move to the 3 Simple Rules - which in our experience is often all that is needed for near-definitive diagnosis. |
==========================
==========================
==========================
Figure 4: The presence of a large upright R
wave in lead aVR during a WCT rhythm is virtually diagnostic of VT (since this
finding implies ventricular activation begins in the apex). Finding a QR
complex or a small amplitude complex (2nd and 3rd examples shown) is
nondiagnostic.
==========================
Selected REFERENCES:
- Brugada P, Brugada J, Mont L, et al: A New Approach to the Differential Diagnosis of a Regular Tachycardia with a Wide QRS Complex. Circulation 83:1649-1659, 1991.
- Blomstrom-Lundqvist C, Scheinman MM, Aliot EM, et al: ACC/AHA/ESC Guidelines for Management of Patients with Supraventricular Arrhythmias- Executive Summary. J Am Coll Cardiol 42:1493-1531, 2003.
- Vereckei A, Duray G, Szenasi G: Application of a New Algorithm in the Differential Diagnosis of Wide QRS Complex Tachycardia. Eur Heart J 28:589-600, 2007.
- Sasaki K: A New Simple Algorithm for Diagnosing Wide QRS Complex Tachycardia: Comparison with Brugada, Vereckei and aVR Algorithms. Circulation 120:S671, 2009.
==========================
- Back to ECG BLOG #42 -
==========================
- Section 06.0 — on Using Adenosine -
- Section 07.0 — on Known VT -
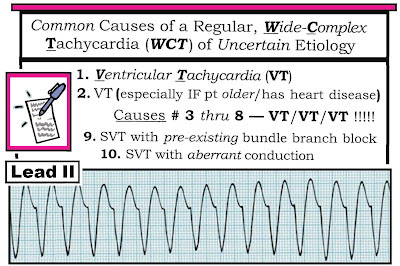
- Sections 08.0, 09.0,10.0 — on The Regular Wide Tachycardia -
- Section 13.0 — on SVT of Uncertain Etiology -
-----------------------------------------------------------------------

.jpg)
.jpg)
.jpg)
No comments:
Post a Comment